It always depends on your documentation.
These codes are by site & measurement of the defect(s).
Modifier 51 is defined as multiple surgeries/procedures.
Multiple surgeries performed on the same day, during the same surgical session.
Diagnostic Imaging Services subject to the Multiple Procedure Payment Reduction that are provided on the same day, during the same session by the same provider.
Note: Medicare doesn’t recommend reporting Modifier 51 on your claim; our processing system will append the modifier to the correct procedure code as appropriate.
Appropriate System Usage
Modifier is appended when:
The same physician performs more than one surgical service at the same session (Indicator 2).
The technical component of multiple diagnostic procedures, Multiple Procedure Payment Reduction (MPPR) rule applies (Indicator 4).
The multiple surgical procedures are done on same day but billed on two separate claims.
The surgical procedure code is the lower physician fee schedule amount.
The diagnostic imaging procedure with the lower technical component fee schedule amount.
Inappropriate System Usage
Do not append to add-on codes (See Appendix D of the CPT manual)
Do not report on all lines of service
Do not append when two or more physicians each perform distinctly, different, unrelated surgeries on the same day to the same patient.

www.novitas-solutions.com
Modifier 59
What you need to know
Under certain circumstances, it may be necessary to indicate that a procedure or service was distinct or independent from other non-evaluation and management (E/M) services performed on the same day. Modifier 59 is used to identify procedures/services, other than E/M services, that are not normally reported together, but are appropriate under the circumstances.
It is the most reported modifier that affects National Correct Coding Initiative (NCCI) processing.
The Medicare NCCI includes edits that define when two HCPCS / CPT codes should not be reported together.
A correct coding modifier indicator (CCMI) of “0,” indicates the codes should never be reported together by the same provider for the same beneficiary on the same date of service. If they are reported on the same date of service, the column one code is eligible for payment and the column two code is denied.
A CCMI of “1,” indicates the codes may be reported together only in defined circumstances, which are identified on the claim using specific NCCI associated modifiers.
CCMI of "9," NCCI editing does not apply.
This modifier may be reported to indicate that a procedure or service was distinct or independent from other services performed on the same day.
Note: Modifier 59 should not be appended to an E/M service.
Report HCPCS modifiers XE, XP, XS, and XU to provide greater reporting specificity in situations where modifier 59 was previously reported. For details on modifiers 59 and X (EPSU, please refer to the
Modifiers 59 and X (EPSU).
Appropriate Uses:
A different session
Different procedure or surgery
Different site or organ system: If two procedures are performed at separate anatomical sites or at separate patient encounters on the same date of service separate incision or excision
Separate lesion, or separate injury (or area in injury in extensive injuries) not ordinarily encountered or performed on the same day by the same individual
Second initial injection procedure when protocol requires two separate sites or when the patient has to come back for a separately identifiable service
Modifiers XE, XS, XP, and XU give greater reporting specificity in situations where you used modifier 59 previously. Use these modifiers instead of modifier 59 whenever possible. (Only use modifier 59 if no other more specific modifier is appropriate.)
For details, including appropriate and inappropriate uses and examples of modifiers 59 and X(EPSU), please refer to the CMS MLN Fact Sheet,
Proper Use of Modifiers 59 & –X{EPSU}
CMS allows the modifiers 59 or –X{ESPU} on Column One or Column Two codes (see the related transmittal at
CR11168).
Evaluate other
anatomical modifiers such as the RT/LT identifying right and left, F1 - F0 to identify fingers, T1-T0 to identify toes and E1-E4 to identify eyelids, coronary arteries modifiers, LC, LD, LM, RC or RI.
Inappropriate Uses:
When another established more descriptive modifier is available and more appropriate.
When used with an E/M service.
If submitted on E/M codes 99201-99499, E/M codes are processed as though a modifier were not present (i.e., the code pair will be subject to NCCI editing and has an indicator that does not allow bypass).
To report a separate and distinct E/M service with a non-E/M service performed on the same date (refer modifier 25).
When a valid modifier exists to identify the services.
When documentation does not support the separate and distinct status.
When used to indicate multiple administration of injections of the same drug.
When the NCCI tables lists the procedure code pair with a modifier indicator of "0".

www.novitas-solutions.com
Appropriate System Usage
Modifier is appended when:
The same physician performs more than one surgical service at the same session (Indicator 2).
The technical component of multiple diagnostic procedures, Multiple Procedure Payment Reduction (MPPR) rule applies (Indicator 4).
The multiple surgical procedures are done on same day but billed on two separate claims.
The surgical procedure code is the lower physician fee schedule amount.
The diagnostic imaging procedure with the lower technical component fee schedule amount.
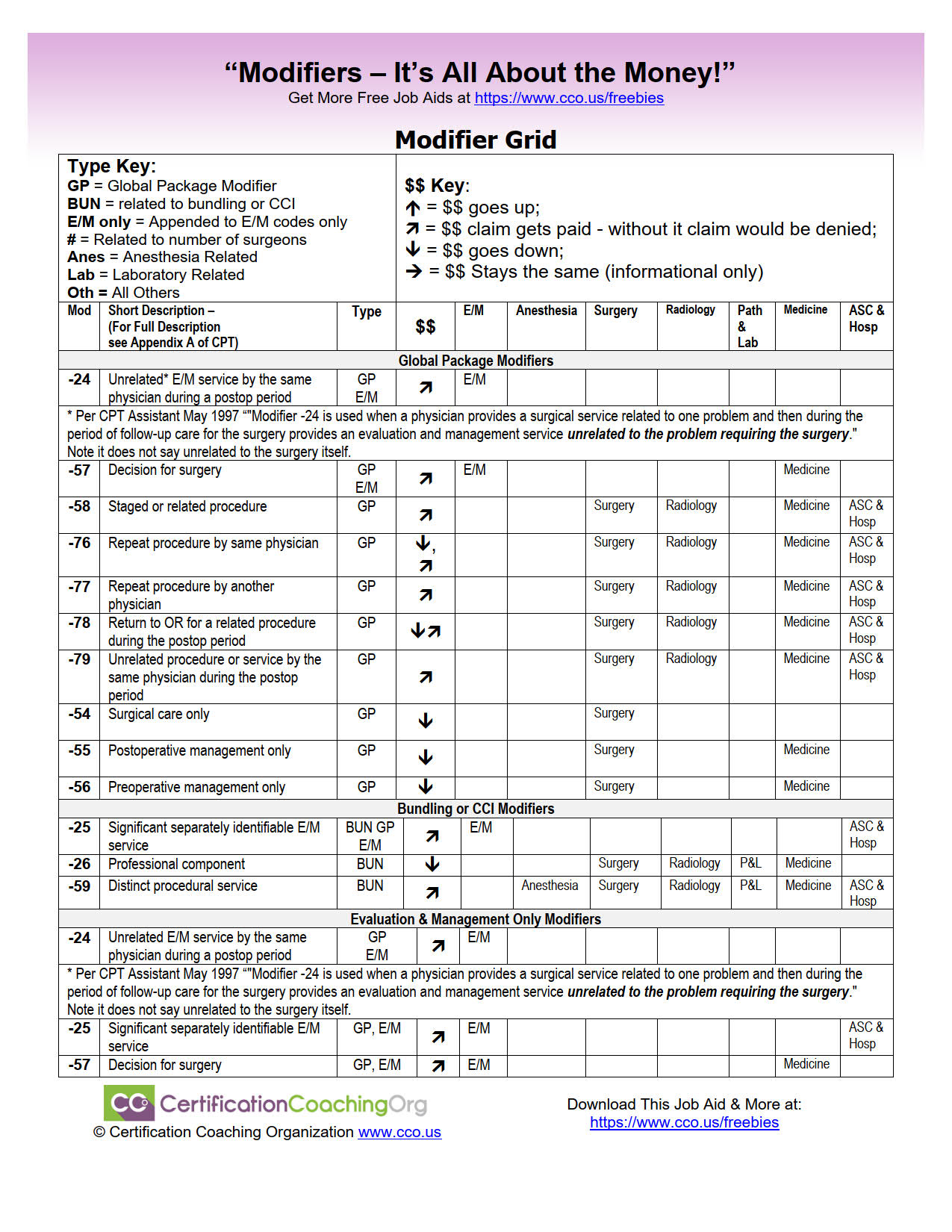
CPT Modifier Decision Grid Tool
CPT Modifier Decision Grid Tool
Are CPT modifiers making you mad? Are you unsure of what CPT modifier code to use? Let us help you navigate the CPT modifier maze with our easy to use, at-a-glance modifier decision grid tool. It provides you with a comprehensive medical billing modifiers list that is sure to make your life easier when it comes to ensuring you are getting the medical coding reimbursement that your practice deserves.
This CPT Modifier Decision Grid Tool will help you to:
- Decide which family of modifiers your should be using
- Help you understand how reimbursement is affected by applying certain modifiers
- See which category in CPT typically uses these modifiers
- Understand when a claim may get denied if a CPT modifier is not attached
- and more…
For instance, did you know that modifier -63 (procedure performed on infants less than 4kg) will increase your reimbursement? And, what if you do not use modifier -57 to denote decision for surgery? Well, your claim could be denied.
Free Job Aid: This CPT Modifier Decision Grid Tool will help you pick the correct CPT Modifiers at your medical coding job.

www.cco.us