I was wondering if anyone had any additional information on learning how to code for anesthesia services in labor and delivery for the Pro-Fee side of things? I have always been doing the Pro-Fee but was mainly in the Internal Medicine side. I was just recently transferred to this work queue and having a tough time with the coding. I'm told to pick up my codes from the H & P from the admitting provider but then I am being told to pick up codes from the Anesthesiologist who did the Pre Visit for the CRNA. Does anyone have any tips or recommendations in this area? Any advice would be greatly appreciated as I am drowning in this work queue. 
Install the app
How to install the app on iOS
Follow along with the video below to see how to install our site as a web app on your home screen.
Note: This feature may not be available in some browsers.
-

Register to Access the Free Forums and 3 Free CEUs!
To view the content for the 3 free CEUs, please sign up today.
CLICK HERE TO REGISTER -
The CCO Community is Moving to Circle!
Click Here to Read More -

Missing Access To A Course, Blitz or Exam? Have Technical Issues? Open a Help Desk Ticket
Please Do Not Post in the Community About Access or Technical Issues
CCO Business Hours for Help Desk and Coaching: Mon-Fri 9am-4pm Eastern
You are using an out of date browser. It may not display this or other websites correctly.
You should upgrade or use an alternative browser.
You should upgrade or use an alternative browser.
Anesthesia Coding
- Thread starter JoT_60483
- Start date
- Status
- Not open for further replies.
Lori
Well-known member
ASA Relative Value Guide (RVG) laid out four recommended options to charge calculation for a labor epidural service, which opened the flood gates for an almost endless number of variations as practices explored ways to optimize the revenue potential of this service. The RVG’s billing options for OB anesthesia, specifically in connection with a labor epidural, are as follows:
An Assortment of Rules
Based on all these CPT coding and RVG billing options, the ABC billing system, First Anesthesia, now includes no less than 20 specific rules for OB billing. The key issue is the determination of time units. Historically, payer policies required the documentation of actual time spent with the patient, but increasingly anesthesia providers feel they should be paid for the time they are available. Diverse payer policies are a critical factor. The goal is to ensure appropriate payment. Usually, the Medicaid policies are the most specific, even though the rates are the lowest. Every state Medicaid policy for OB anesthesia is different.
Obviously, one of the major distinctions between surgical anesthesia and obstetric anesthesia is the fact that one provider may be managing multiple epidurals simultaneously. For most payers this is not an issue, but the rules for MediCal (Medicaid in California) take concurrency into consideration. The total units billed per hour cannot be more than four, no matter how many epidurals an anesthesiologist may be managing at one time even those that are not MediCal patients. This unique rule requires that we undertake a special review and calculation of concurrency for each labor epidural service, which in turn has necessitated some fairly complicated programming of our system.
Validating the accuracy of payments has become a significant challenge when it comes to OB anesthesia. Ironically, it is the lowest paying plans, mainly the Medicaid and Medicaid Managed Care plans, that require the most careful monitoring.
 www.anesthesiallc.com
www.anesthesiallc.com
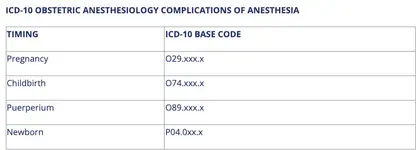
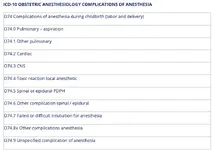
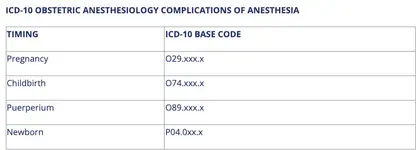
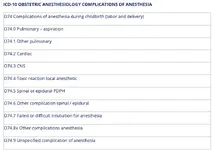
Complications of obstetric anesthesia are coded by pregnancy (O29), childbirth (O74) or puerperium (O94). Events beyond the 6-week puerperium are coded as non-obstetric. Complications of anesthesia are defined in ICD-10 as pulmonary, cardiac, CNS, toxic reaction to local anesthetic, spinal epidural, post-dural puncture headache (PDPH), other complications of spinal epidural, failure or difficult intubation of anesthesia, other complications of anesthesia, and unspecified complications of anesthesia.
Payment for anesthesia services rendered during labor is calculated differently from that for other anesthesia services. Payment is made according to the unit values listed on the tables below. The global unit values shown on the table shown on the table represent a combination of the base units for anesthesia rendered during labor and time units.

For each additional hour beyond three, one more unit will be allowed. Thus, four hours would be valued at 14 units, five hours at 15 units, six hours at 16 units and so on. A maximum number of units will not be imposed, as long as services are still being rendered.
 prc.hmsa.com
prc.hmsa.com
- Base units, plus minutes from insertion of catheter to delivery, subject to a reasonable cap.
- Base units, plus one unit per hour plus direct contact time.
- Incremental time-based fees.
- Flat fee.
- 01960 Anesthesia for vaginal delivery only, no mention of epidural (5 units)
- 01961 Anesthesia for cesarean section, no mention of epidural (7 units)
- 01967 Epidural for labor analgesia (5 units)
- 01968 Epidural for cesarean section after epidural (Add-on code worth 3 units*)
An Assortment of Rules
Based on all these CPT coding and RVG billing options, the ABC billing system, First Anesthesia, now includes no less than 20 specific rules for OB billing. The key issue is the determination of time units. Historically, payer policies required the documentation of actual time spent with the patient, but increasingly anesthesia providers feel they should be paid for the time they are available. Diverse payer policies are a critical factor. The goal is to ensure appropriate payment. Usually, the Medicaid policies are the most specific, even though the rates are the lowest. Every state Medicaid policy for OB anesthesia is different.
Obviously, one of the major distinctions between surgical anesthesia and obstetric anesthesia is the fact that one provider may be managing multiple epidurals simultaneously. For most payers this is not an issue, but the rules for MediCal (Medicaid in California) take concurrency into consideration. The total units billed per hour cannot be more than four, no matter how many epidurals an anesthesiologist may be managing at one time even those that are not MediCal patients. This unique rule requires that we undertake a special review and calculation of concurrency for each labor epidural service, which in turn has necessitated some fairly complicated programming of our system.
Validating the accuracy of payments has become a significant challenge when it comes to OB anesthesia. Ironically, it is the lowest paying plans, mainly the Medicaid and Medicaid Managed Care plans, that require the most careful monitoring.
OB Anesthesia: A Special Challenge for Anesthesia Practices | Anesthesia Business Consultants
ABC eAlerts are timely updates and news affecting anesthesia and pain management providers.
Complications of obstetric anesthesia are coded by pregnancy (O29), childbirth (O74) or puerperium (O94). Events beyond the 6-week puerperium are coded as non-obstetric. Complications of anesthesia are defined in ICD-10 as pulmonary, cardiac, CNS, toxic reaction to local anesthetic, spinal epidural, post-dural puncture headache (PDPH), other complications of spinal epidural, failure or difficult intubation of anesthesia, other complications of anesthesia, and unspecified complications of anesthesia.
Payment for anesthesia services rendered during labor is calculated differently from that for other anesthesia services. Payment is made according to the unit values listed on the tables below. The global unit values shown on the table shown on the table represent a combination of the base units for anesthesia rendered during labor and time units.

For each additional hour beyond three, one more unit will be allowed. Thus, four hours would be valued at 14 units, five hours at 15 units, six hours at 16 units and so on. A maximum number of units will not be imposed, as long as services are still being rendered.
Provider Resource Center
MaxJ_73339
New member
Thanks for the information, however, it's hard to understand it. 
MaxJ_73339
New member
You'll be able to collect a lot of information from the links mentioned above.Wow! That is a lot of information!! I will have to look at the links you provided and see what all those are saying also. Now my mind is really blown! LOL
Did you have all of this info in your notes or did you just write that up now? That is very good!!
Lori
Well-known member
Wow! That is a lot of information!! I will have to look at the links you provided and see what all those are saying also. Now my mind is really blown! LOL
Did you have all of this info in your notes or did you just write that up now? That is very good!!
My specialty is finding resources to back up what I want you to know (CCO & others may have already answered this question with YT or articles such as the links provided) or think you would find useful concerning the question posted to the best of my ability.
The excerpts & pics are what I feel address your question most.
Some things are more difficult to explain than others lol.
You may also find this thread useful:
Resource - Anesthesia Coding
Anesthesiology coding is a unique specialty within the world of medical coding, and it requires a special skill-set and mastery of both the CPT coding paradigm and the ASA coding system. They must know surgical and obstetric coding rules in addition to the anesthesiology regulations. Add to that...
- Status
- Not open for further replies.
