Anesthesiology coding is a unique specialty within the world of medical coding, and it requires a special skill-set and mastery of both the CPT coding paradigm and the ASA coding system. They must know surgical and obstetric coding rules in addition to the anesthesiology regulations. Add to that the expertise needed to code pain management procedures which encompasses E&M services, radiology, and surgical coding, and you have a very esoteric job description requiring advanced anesthesia coding training, mentoring, hands-on experience, and continuous updating and supervision
Anesthesia
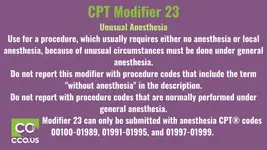
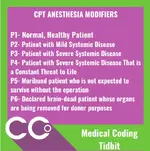
— Anesthesia is a state of temporary induced (Drug/Gas) loss of sensation or awareness. The CPT code range from 00100 – 01999 plus “Anesthesia modifier”.
— An Anesthesiologist, Anesthesia assistant or qualified non-physician anesthetist can provide Anesthesia service.
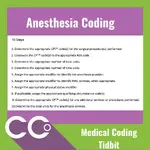
The anesthesia care package consists of preoperative evaluation, standard preparation and monitoring services, administration of anesthesia, and post-anesthesia recovery care.
Included services
1. Preoperative & Postoperative care
2. Administration of fluids and/or Blood
3. Monitoring services (Eg: BP, Temperature, ECG, Oximetry, Mass Spectrometry, and Capnography)
Excluded services
1. Other Monitoring services like Central venous, Intra-arterial and Swan-Ganz
Types of Anesthesia:
General
Regional
Topical or Local
(General anesthesia suppresses the CNS, Regional and local anesthesia block transmission of nerve impulses)
Analgesia/Deep Sedation
Anesthesia
— Anesthesia is a state of temporary induced (Drug/Gas) loss of sensation or awareness. The CPT code range from 00100 – 01999 plus “Anesthesia modifier”.
— An Anesthesiologist, Anesthesia assistant or qualified non-physician anesthetist can provide Anesthesia service.
The anesthesia care package consists of preoperative evaluation, standard preparation and monitoring services, administration of anesthesia, and post-anesthesia recovery care.
Included services
1. Preoperative & Postoperative care
2. Administration of fluids and/or Blood
3. Monitoring services (Eg: BP, Temperature, ECG, Oximetry, Mass Spectrometry, and Capnography)
Excluded services
1. Other Monitoring services like Central venous, Intra-arterial and Swan-Ganz
Types of Anesthesia:
General
- Beneficiary is drug-induced by mask or IV to a loss of consciousness and are not awakened, even by painful stimulation
- Many functions of the body will slow down or need help to work effectively; a tube may be placed to assist the beneficiary with breathing
- Heart rate, blood pressure, breathing and other vital signs are monitored
- Services include:
- Pre/post-operative visits
- Administration of fluids and/or blood
- Usual monitoring service (e.g., temperature, ECG, blood pressure, oximetry, capnography and mass spectrometry)
Regional
- May be performed as a single injection or with a continuous catheter in which medication is given over a prolonged period (includes epidurals, spinals and other central nerve blocks)
- Medication delivered to specific level of the spinal cord and/or peripheral nerves
- Used when loss of consciousness is not desired by a sufficient loss of movement is required
Topical or Local
- Drug application or injection or a combination of drugs
- Stops or prevents painful sensation to specific area
- Not payable by Medicare (bundled into service performed)
(General anesthesia suppresses the CNS, Regional and local anesthesia block transmission of nerve impulses)
Analgesia/Deep Sedation
- Analgesic drugs act in various ways on the peripheral and central nervous systems to give pain relief without losing consciousness
- Patient-controlled analgesia not payable by Medicare
- Airway intervention may be required
- Non-anesthesia physicians can bill if credentialed, properly trained, etc.
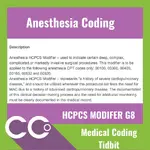
- Modifier G8 must be appended: Monitored anesthesia care for deep complex, complicated or markedly invasive surgical procedure
- Drug-induced consciousness with no intervention required to maintain airways; however, cardiovascular is maintained
- Beneficiary oxygenation, ventilation, circulation and temperature should be evaluated. Close monitoring is necessary to anticipate the need for general anesthesia administration or for the treatment of adverse physiologic reactions
- By practitioner qualified to administer anesthesia defined by Code of Federal Regulations 42 CFR 482.52(a)
- Deep sedation/analgesia included in MAC and beneficiary can still respond
- Drug-induced depression of consciousness where beneficiaries become relaxed and insensitive to pain but remain awake and able to respond to verbal instruction
- No interventions are required to maintain airway; Cardiovascular function is usually maintained
- Does not include deep or minimal sedation or MAC
- Physician or a face-to-face supervised specially trained sedation nurse may perform
- Must have independent trained observer, for example, Nurse Practitioner (NP), Physician Assistant (PA), Registered Nurse (RN), whose sole duty is to monitor beneficiary's level of consciousness and physiological status; must be present throughout entire diagnostic or therapeutic service; must be identified in notes with credentials
- Time ends at conclusion of personal contact by physician providing sedation