When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source.
The ICD-10-CM guidelines state that if the cause of the pain is known, you should assign a code for the underlying diagnosis, not the pain code.
Only report pain diagnosis codes from the G89 category as the primary diagnosis when:
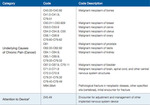
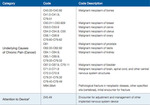
Types of Pain Codes
You can find pain codes in three different places in the ICD-10-CM manual:
Chronic pain syndrome is chronic pain associated with significant psychosocial dysfunction. The psychosocial problems may include depression, drug dependence, complaints that are out of proportion to the physical findings, anxiety, and other manifestations. Chronic pain syndrome is not synonymous with chronic pain. You should code this condition only when the physician specifically documents it. Chronic pain syndrome is reported with code G89.4 (Chronic pain syndrome).
b. Pain - Category G89
1) General coding information
Codes in category G89, Pain, not elsewhere classified, may be used in
conjunction with codes from other categories and chapters to provide
more detail about acute or chronic pain and neoplasm-related pain,
unless otherwise indicated below.
If the pain is not specified as acute or chronic, post-thoracotomy,
postprocedural, or neoplasm-related, do not assign codes from category
G89.
A code from category G89 should not be assigned if the underlying
(definitive) diagnosis is known, unless the reason for the encounter is
pain control/ management and not management of the underlying
condition.
When an admission or encounter is for a procedure aimed at treating the
underlying condition (e.g., spinal fusion, kyphoplasty), a code for the
underlying condition (e.g., vertebral fracture, spinal stenosis) should be
assigned as the principal diagnosis. No code from category G89 should
be assigned.
(a) Category G89 Codes as Principal or First-Listed Diagnosis
Category G89 codes are acceptable as principal diagnosis or the
first-listed code:
• When pain control or pain management is the reason for the
admission/encounter (e.g., a patient with displaced
intervertebral disc, nerve impingement and severe back pain
presents for injection of steroid into the spinal canal). The
underlying cause of the pain should be reported as an
additional diagnosis, if known.
• When a patient is admitted for the insertion of a
neurostimulator for pain control, assign the appropriate pain
code as the principal or first-listed diagnosis. When an
ICD-10-CM Official Guidelines for Coding andReporting
FY 2023
Page 45 of 118
admission or encounter is for a procedure aimed at treating
the underlying condition and a neurostimulator is inserted for
pain control during the same admission/encounter, a code for
the underlying condition should be assigned as the principal
diagnosis and the appropriate pain code should be assigned as
a secondary diagnosis.
(b) Use of Category G89 Codes in Conjunction with Site Specific
Pain Codes
(i) Assigning Category G89 and Site-Specific Pain Codes
Codes from category G89 may be used in conjunction
with codes that identify the site of pain (including codes
from chapter 18) if the category G89 code provides
additional information. For example, if the code describes
the site of the pain, but does not fully describe whether
the pain is acute or chronic, then both codes should be
assigned.
(ii) Sequencing of Category G89 Codes with Site-Specific
Pain Codes
The sequencing of category G89 codes with site- specific
pain codes (including chapter 18 codes), is dependent on
the circumstances of the encounter/admission as follows:
• If the encounter is for pain control or pain
management, assign the code from category G89
followed by the code identifying the specific site
of pain (e.g., encounter for pain management for
acute neck pain from trauma is assigned code
G89.11, Acute pain due to trauma, followed by
code M54.2, Cervicalgia, to identify the site of
pain).
• If the encounter is for any other reason except pain
control or pain management, and a related
definitive diagnosis has not been established
(confirmed) by the provider, assign the code for
the specific site of pain first, followed by the
appropriate code from category G89.
2) Pain due to devices, implants and grafts
See Section I.C.19. Pain due to medical devices
3) Postoperative Pain
The provider’s documentation should be used to guide the coding of
postoperative pain, as well as Section III. Reporting Additional
Diagnoses and Section IV. Diagnostic Coding and Reporting in the
Outpatient Setting.
ICD-10-CM Official Guidelines for Coding andReporting
FY 2023
Page 46 of 118
The default for post-thoracotomy and other postoperative pain not
specified as acute or chronic is the code for the acute form.
Routine or expected postoperative pain immediately after surgery should
not be coded.
(a) Postoperative pain not associated with specific postoperative
complication
Postoperative pain not associated with a specific postoperative
complication is assigned to the appropriate postoperative pain
code in category G89.
(b) Postoperative pain associated with specific postoperative
complication
Postoperative pain associated with a specific postoperative
complication (such as painful wire sutures) is assigned to the
appropriate code(s) found in Chapter 19, Injury, poisoning, and
certain other consequences of external causes. If appropriate, use
additional code(s) from category G89 to identify acute or chronic
pain (G89.18 or G89.28).
4) Chronic pain
Chronic pain is classified to subcategory G89.2. There is no time frame
defining when pain becomes chronic pain. The provider’s documentation
should be used to guide use of these codes.
5) Neoplasm Related Pain
Code G89.3 is assigned to pain documented as being related, associated
or due to cancer, primary or secondary malignancy, or tumor. This code
is assigned regardless of whether the pain is acute or chronic.
This code may be assigned as the principal or first-listed code when the
stated reason for the admission/encounter is documented as pain
control/pain management. The underlying neoplasm should be reported
as an additional diagnosis.
When the reason for the admission/encounter is management of the
neoplasm and the pain associated with the neoplasm is also documented,
code G89.3 may be assigned as an additional diagnosis. It is not
necessary to assign an additional code for the site of the pain.
See Section I.C.2. for instructions on the sequencing of neoplasms for all
other stated reasons for the admission/encounter (except for pain
control/pain management).
ICD-10-CM Official Guidelines for Coding andReporting
FY 2023
Page 47 of 118
6) Chronic pain syndrome
Central pain syndrome (G89.0) and chronic pain syndrome (G89.4) are
different than the term “chronic pain,” and therefore codes should only
be used when the provider has specifically documented this condition.
See Section I.C.5. Pain disorders related to psychological factors
 www.aapc.com
www.aapc.com
 www.outsourcestrategies.com
www.outsourcestrategies.com


The ICD-10-CM guidelines state that if the cause of the pain is known, you should assign a code for the underlying diagnosis, not the pain code.
Only report pain diagnosis codes from the G89 category as the primary diagnosis when:
- The acute or chronic pain and neoplasm pain provide more detail when used with codes from other categories; or
- The reason for the service is for pain control or pain management.
Types of Pain Codes
You can find pain codes in three different places in the ICD-10-CM manual:
- Pain that points to a disorder of a specific body system is classified in the body system chapters. For example, low back pain is classified in the Musculoskeletal chapter (M54.5) and testicular pain is classified in the Genitourinary System chapter (N50.8).
- Pain that does not point to a specific body system is classified in the Symptoms and Signs chapter. For example, abdominal pain is classified to category R10.
- Certain specific types of pain are classified to category G89 (Pain, not elsewhere classified) in the Nervous System chapter
Chronic pain syndrome is chronic pain associated with significant psychosocial dysfunction. The psychosocial problems may include depression, drug dependence, complaints that are out of proportion to the physical findings, anxiety, and other manifestations. Chronic pain syndrome is not synonymous with chronic pain. You should code this condition only when the physician specifically documents it. Chronic pain syndrome is reported with code G89.4 (Chronic pain syndrome).
b. Pain - Category G89
1) General coding information
Codes in category G89, Pain, not elsewhere classified, may be used in
conjunction with codes from other categories and chapters to provide
more detail about acute or chronic pain and neoplasm-related pain,
unless otherwise indicated below.
If the pain is not specified as acute or chronic, post-thoracotomy,
postprocedural, or neoplasm-related, do not assign codes from category
G89.
A code from category G89 should not be assigned if the underlying
(definitive) diagnosis is known, unless the reason for the encounter is
pain control/ management and not management of the underlying
condition.
When an admission or encounter is for a procedure aimed at treating the
underlying condition (e.g., spinal fusion, kyphoplasty), a code for the
underlying condition (e.g., vertebral fracture, spinal stenosis) should be
assigned as the principal diagnosis. No code from category G89 should
be assigned.
(a) Category G89 Codes as Principal or First-Listed Diagnosis
Category G89 codes are acceptable as principal diagnosis or the
first-listed code:
• When pain control or pain management is the reason for the
admission/encounter (e.g., a patient with displaced
intervertebral disc, nerve impingement and severe back pain
presents for injection of steroid into the spinal canal). The
underlying cause of the pain should be reported as an
additional diagnosis, if known.
• When a patient is admitted for the insertion of a
neurostimulator for pain control, assign the appropriate pain
code as the principal or first-listed diagnosis. When an
ICD-10-CM Official Guidelines for Coding andReporting
FY 2023
Page 45 of 118
admission or encounter is for a procedure aimed at treating
the underlying condition and a neurostimulator is inserted for
pain control during the same admission/encounter, a code for
the underlying condition should be assigned as the principal
diagnosis and the appropriate pain code should be assigned as
a secondary diagnosis.
(b) Use of Category G89 Codes in Conjunction with Site Specific
Pain Codes
(i) Assigning Category G89 and Site-Specific Pain Codes
Codes from category G89 may be used in conjunction
with codes that identify the site of pain (including codes
from chapter 18) if the category G89 code provides
additional information. For example, if the code describes
the site of the pain, but does not fully describe whether
the pain is acute or chronic, then both codes should be
assigned.
(ii) Sequencing of Category G89 Codes with Site-Specific
Pain Codes
The sequencing of category G89 codes with site- specific
pain codes (including chapter 18 codes), is dependent on
the circumstances of the encounter/admission as follows:
• If the encounter is for pain control or pain
management, assign the code from category G89
followed by the code identifying the specific site
of pain (e.g., encounter for pain management for
acute neck pain from trauma is assigned code
G89.11, Acute pain due to trauma, followed by
code M54.2, Cervicalgia, to identify the site of
pain).
• If the encounter is for any other reason except pain
control or pain management, and a related
definitive diagnosis has not been established
(confirmed) by the provider, assign the code for
the specific site of pain first, followed by the
appropriate code from category G89.
2) Pain due to devices, implants and grafts
See Section I.C.19. Pain due to medical devices
3) Postoperative Pain
The provider’s documentation should be used to guide the coding of
postoperative pain, as well as Section III. Reporting Additional
Diagnoses and Section IV. Diagnostic Coding and Reporting in the
Outpatient Setting.
ICD-10-CM Official Guidelines for Coding andReporting
FY 2023
Page 46 of 118
The default for post-thoracotomy and other postoperative pain not
specified as acute or chronic is the code for the acute form.
Routine or expected postoperative pain immediately after surgery should
not be coded.
(a) Postoperative pain not associated with specific postoperative
complication
Postoperative pain not associated with a specific postoperative
complication is assigned to the appropriate postoperative pain
code in category G89.
(b) Postoperative pain associated with specific postoperative
complication
Postoperative pain associated with a specific postoperative
complication (such as painful wire sutures) is assigned to the
appropriate code(s) found in Chapter 19, Injury, poisoning, and
certain other consequences of external causes. If appropriate, use
additional code(s) from category G89 to identify acute or chronic
pain (G89.18 or G89.28).
4) Chronic pain
Chronic pain is classified to subcategory G89.2. There is no time frame
defining when pain becomes chronic pain. The provider’s documentation
should be used to guide use of these codes.
5) Neoplasm Related Pain
Code G89.3 is assigned to pain documented as being related, associated
or due to cancer, primary or secondary malignancy, or tumor. This code
is assigned regardless of whether the pain is acute or chronic.
This code may be assigned as the principal or first-listed code when the
stated reason for the admission/encounter is documented as pain
control/pain management. The underlying neoplasm should be reported
as an additional diagnosis.
When the reason for the admission/encounter is management of the
neoplasm and the pain associated with the neoplasm is also documented,
code G89.3 may be assigned as an additional diagnosis. It is not
necessary to assign an additional code for the site of the pain.
See Section I.C.2. for instructions on the sequencing of neoplasms for all
other stated reasons for the admission/encounter (except for pain
control/pain management).
ICD-10-CM Official Guidelines for Coding andReporting
FY 2023
Page 47 of 118
6) Chronic pain syndrome
Central pain syndrome (G89.0) and chronic pain syndrome (G89.4) are
different than the term “chronic pain,” and therefore codes should only
be used when the provider has specifically documented this condition.
See Section I.C.5. Pain disorders related to psychological factors
Pain: ICD-10-CM Coding
When seeking a pain diagnosis, identify as precisely as possible the pain’s location and/or source.
Appropriate Use of Category G89 Codes in ICD-10
The ICD-10 coding of acute or chronic pain involves the codes under category G89. This article explores how to use those codes properly.
 www.outsourcestrategies.com
www.outsourcestrategies.com